Does Daily Movement Help or Harm Your Knees?
Let’s clear up the confusion by delving into what the meniscus is and what it does, surgical and non-surgical approaches to a meniscus tear, plus how physiotherapy can benefit meniscus injury management.
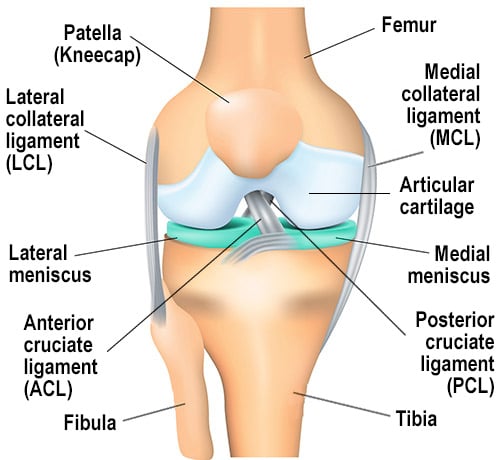
Meniscus Anatomy
The meniscus is a fibrocartilage structure that sits between the femur (thigh bone) and the tibia (shin bone). Each knee has two menisci – the medial meniscus (inner side of the knee) and the lateral meniscus (outer side of the knee) – and they play a crucial role in the knee’s functionality.
Shock Absorption
The meniscus helps distribute forces across the knee joint when walking, jumping, landing, running, or changing direction.
Lubrication
The meniscus helps to move and distribute synovial fluid, which lubricates the joint and delivers nutrients to the cartilage.
Joint Stability
The meniscus deepens the contact area within the knee, providing greater mechanical stability to the joint.
Proprioception
The meniscus contains mechanoreceptors that help your brain detect joint position and movement.
Meniscus = Sponge
Movement is essential for maintaining good health because it promotes proper function of the body’s systems, improves circulation, strengthens muscles, and boosts overall well-being.
For example, imagine a kitchen sponge sitting dry on your sink. It’s brittle and hard to use. However, once soaked and compressed for use, it becomes hydrated, resilient, soft, and easy to work with.
But if you are not using your “sponge”, then it could look and feel a little worse for wear.

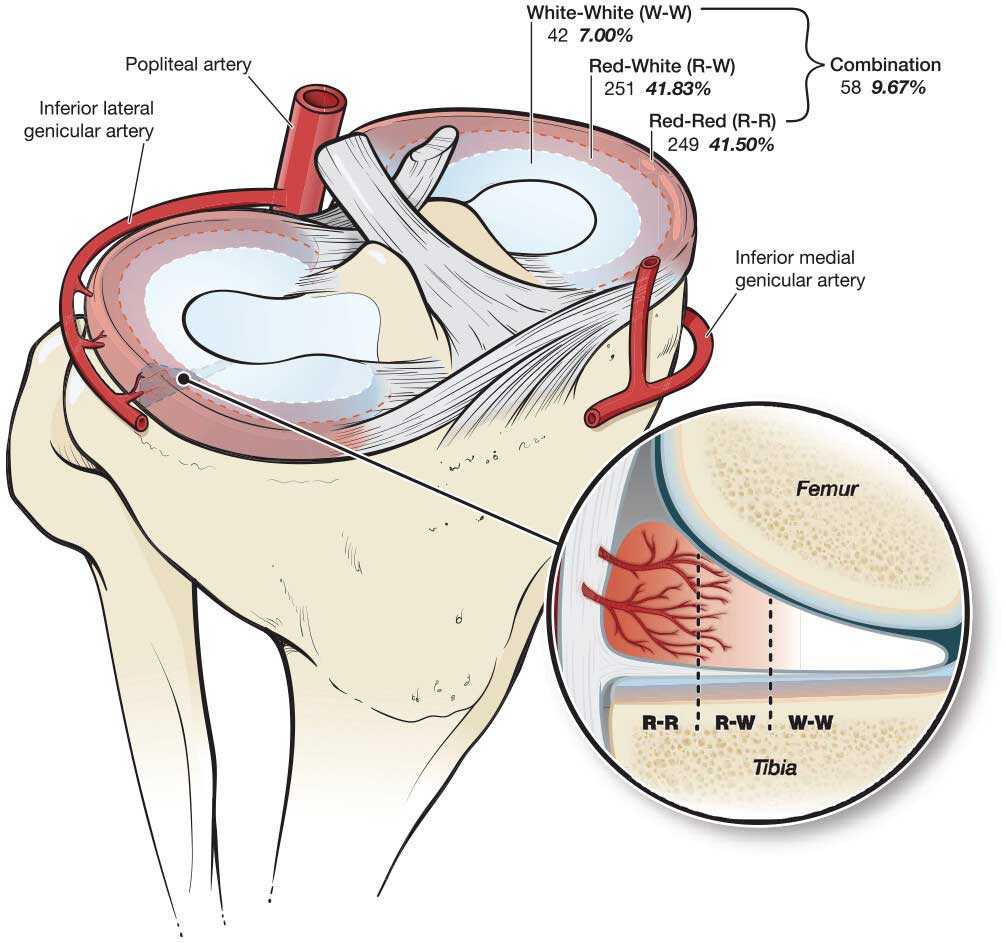
The meniscus anatomy has a limited blood supply, which is why it can be slow to heal after an injury. It’s divided into three zones based on how much blood reaches them:
Red-Red Zone
The outer edge of the meniscus. This area has a rich blood supply, enabling the best possible healing potential and access for meniscus damage treatment.
Red-White Zone
The middle section. It has only a limited blood supply, so meniscus damage treatment and healing are slower.
White-White Zone
The innermost part. It has no blood supply (avascular), making meniscus damage treatment very difficult.
The meniscus anatomy has little to no blood supply, so it relies on nutrients from the synovial fluid. These nutrients are delivered through joint movement — the compressing and releasing of the meniscus. Without regular movement, the meniscus is starved of nourishment and becomes like a brittle sponge, making it more prone to degeneration and tears, requiring meniscus damage treatment.
Surgical vs Non-Surgical Management
Not all meniscus tears are the same, and most do not require surgery. Research has shown no significant difference in functional outcomes between surgery and physiotherapy management for many types of tears.
Surgery is often recommended in cases of mechanical blockage, complex or unstable tears, or when conservative treatment has failed.
Physiotherapists play a vital role in both meniscus damage treatment pathways:
- Prehab before surgery to improve post-operative recovery
- Rehab after surgery to restore mobility, strength, and function
- Conservative management focusing on progressive loading, pain management, and a safe return to activity
How can Physiotherapy help with Meniscus Injury Management?
Assessment
Our approach at Health on Grange Physiotherapy begins with a thorough assessment, which involves listening to your story, understanding your symptoms and goals, and conducting detailed knee tests to evaluate movement, strength, and function. If we suspect a significant tear, we’ll guide you on whether scans or an orthopaedic opinion are needed.
Education
Next comes education and helping you understand your meniscus anatomy, its healing potential, what to expect in recovery, and why loading (done right) is more effective than long-term rest.
Progressive Loading
We then move into progressive loading, finding your optimal starting point and building strength, stability, and confidence step by step.
What to avoid
We’ll also teach you what to avoid when your meniscus is ‘angry’ — like deep squats, twisting or pivoting, high-impact activities, and kneeling or crossing your legs — so you can protect it while it heals.
Your Meniscus is built to move, not to rest
Respect pain, adjust your loads, and keep moving smartly and progressively. Our physiotherapists at Health on Grange Physiotherapy will design a recovery plan tailored to you based on your symptoms, goals, and lifestyle, not just your scan results.
If you’ve noticed a twinge in your knee or your scan mentions degeneration, remember the sponge analogy: movement keeps it healthy!
Let us help you keep your knees healthy and strong — book your appointment today.
References:
Bricca, A., Juhl, C. B., Steultjens, M., Wirth, W., & Roos, E. M. (2019). Impact of exercise on articular cartilage in people at risk of, or with established, knee osteoarthritis: a systematic review of randomised controlled trials. British journal of sports medicine, 53(15), 940-947.
https://www.hss.edu/health-library/conditions-and-treatments/list/meniscus-tear
Kohde, Matthew S., et al. “Age, sex, and BMI differences related to repairable meniscal tears in pediatric and adolescent patients.” The American journal of sports medicine, 51.2 (2023: 389-397.
