In this post, we’ll cover all the key points about Achilles tendinopathy, including its pathology, diagnosis, assessment, and management. Let’s dive in!
What Is Achilles Tendinopathy?
Achilles tendinopathy occurs when the collagen fibres in the Achilles tendon become disorganised. Imagine the tendon like a bundle of uncooked spaghetti, with each strand representing a collagen fibre (photo below). Normally, these fibres line up neatly, working together to transmit force from your muscles to your bones, helping you move.
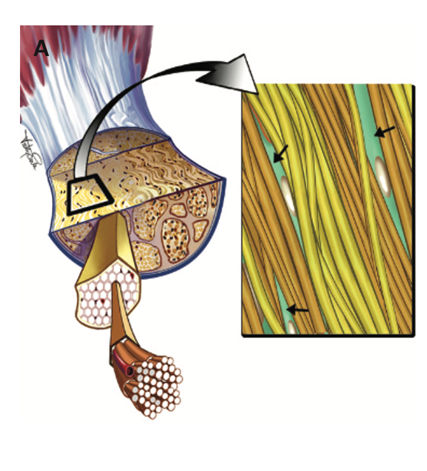
However, when the tendon is overloaded, things start to go wrong. Some fibres no longer run parallel, and others might be lost altogether, making the tendon less effective at transmitting force. As a result, activities like walking, running, or jumping become more difficult.
How Is Achilles Tendinopathy Diagnosed?
Achilles tendinopathy is typically diagnosed based on your symptoms. Localised pain, swelling, and reduced function are key signs (Malliaras, 2022). There are two types of Achilles tendinopathy: insertional (near the heel) and mid-portion (further up the tendon) (photo below). The location of your pain can help determine which type you may have.

Although an ultrasound can be used to diagnose this condition, it’s not always necessary. Clinical assessment is usually enough. In fact, ultrasound findings alone can be misleading, as many people without pain also show tendon changes on scans (Lieberthal et al., 2019). So, the focus should be on your symptoms, not just what the scan shows.
Achilles tendinopathy often occurs after a sudden increase in activity, like when people start running after a break, or athletes return to sport after time off. Lifestyle factors like diabetes, menopause, smoking, and poor sleep can also increase your risk.
What to Expect During a Physiotherapy Assessment
When you come to our clinic, there are six key things we’ll assess:
1. Observation – We’ll look for visible swelling in your Achilles tendon.
2. Palpation – We’ll gently press on your tendon to see if it reproduces your pain.

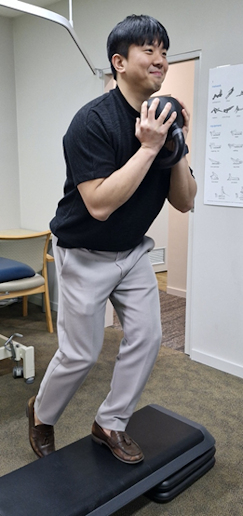
3. Capability Assessments – We’ll check how much load your tendon can handle. This is crucial for planning your treatment.
It would normally include:
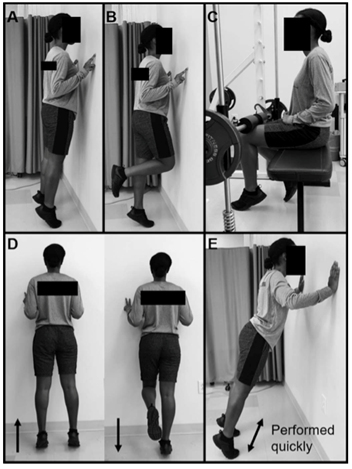
a) Double leg calf raise:
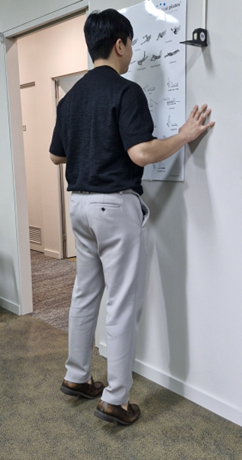
b) Single leg calf raise:
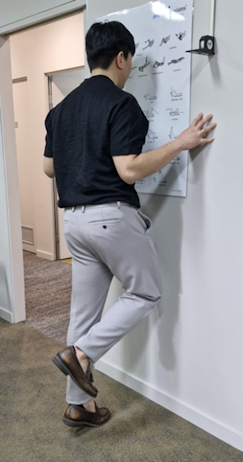
c) Pulsating double and single leg calf raise
i. The same as above, but you perform the movements more rapidly
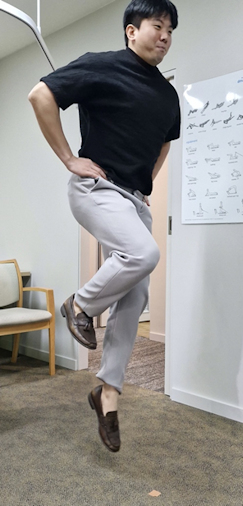
d) Double and Single leg hopping
4. Strength – We’ll test the strength of your calf muscles, especially the gastrocnemius and soleus. They’ll be assessed separately because they work slightly differently.

5. Muscular Power – We’ll evaluate your calf power, which is often neglected but essential for full recovery, especially for athletes. Hopping tests are commonly used to assess muscular power of the calf.
The hopping test has several variations. The single leg hop test measures how far you can hop on each leg, allowing you to compare the performance between your left and right legs to spot any discrepancies. The same approach applies to other variations, like the lateral hop test, triple hop test, or crossover hop test, where you assess different aspects of your muscular power and function.

6. Kinetic Chain – We’ll assess other muscles in your legs, like your glutes and hamstrings, to ensure your Achilles isn’t overloaded due to weaknesses elsewhere.
How Is Achilles Tendinopathy Managed?
Injections – any injections aren’t recommended due to limited evidence supporting it (Silbernagel, Hanlon, & Sprague, 2020). Furthermore, it may harm your tendon in the long run as they negatively affect the cells inside your tendon. Therefore, it’s more important to focus on the healthy parts of your tendon, as research shows there are often plenty of strong collagen fibres still in place even in the presence of tendinopathy (Docking & Cook, 2016).
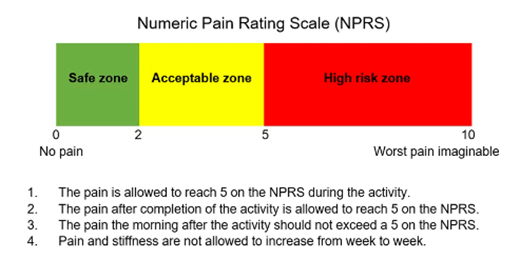
Load Management – The most important part of managing tendinopathy is controlling the load on your tendon. We use a pain-monitoring model to guide you (photo below). Pain that’s tolerable (green light or yellow light) during activity is okay, but if your pain becomes intolerable (red light), or worsens at night or in the following morning, it’s a sign to back off.
Exercise Therapy – Strength and power deficits need to be addressed with a targeted exercise program. This is key to improving your function and avoiding ongoing problems. Research also suggests the exercise has to be high intensity (high load, low repetitions) to generate ideal structural changes inside the tendon (Bohm, Mersmann, & Arampatzis, 2015).
You may also be curious about how long you would need to do the rehabilitation. Research suggests at least 12 weeks of rehabilitation is required for your tendon (Bohm et al., 2015). You would probably feel better within a few weeks, but please do not stop your rehabilitation as it is not enough time for your tendon to get stronger.
What About Other Treatments?
Things like icing, acupuncture, and manual therapy might help with pain relief, but they will not fix your problem. The real focus should be on load management and exercise.
Need Help with Achilles Tendinopathy?
If you or someone you know is dealing with Achilles tendinopathy, don’t hesitate to reach out to us at Health on Grange Physiotherapy. Our team is ready to help you get back on your feet and moving pain-free. Feel free to share this post to help others better understand tendinopathy and promote better care!
References:
Bohm, S., Mersmann, F., & Arampatzis, A. (2015). Human tendon adaptation in response to mechanical loading: a systematic review and meta-analysis of exercise intervention studies on healthy adults. Sports Med Open, 1(1), 7. doi:10.1186/s40798-015-0009-9
Docking, S. I., & Cook, J. (2016). Pathological tendons maintain sufficient aligned fibrillar structure on ultrasound tissue characterization (UTC). Scand J Med Sci Sports, 26(6), 675-683. doi:10.1111/sms.12491
Grävare Silbernagel, K., & Crossley, K. M. (2015). A Proposed Return-to-Sport Program for Patients With Midportion Achilles Tendinopathy: Rationale and Implementation. Journal of Orthopaedic & Sports Physical Therapy, 45(11), 876-886. doi:10.2519/jospt.2015.5885
Khan, K. M., & Scott, A. (2009). Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. Br J Sports Med, 43(4), 247-252. doi:10.1136/bjsm.2008.054239
Lieberthal, K., Paterson, K. L., Cook, J., Kiss, Z., Girdwood, M., & Bradshaw, E. J. (2019). Prevalence and factors associated with asymptomatic Achilles tendon pathology in male distance runners. Phys Ther Sport, 39, 64-68. doi:10.1016/j.ptsp.2019.06.006
Malliaras, P. (2022). Physiotherapy management of Achilles tendinopathy. Journal of Physiotherapy, 68(4), 221-237. doi:https://doi.org/10.1016/j.jphys.2022.09.010
Silbernagel, K. G., Hanlon, S., & Sprague, A. (2020). Current Clinical Concepts: Conservative Management of Achilles Tendinopathy. J Athl Train, 55(5), 438-447. doi:10.4085/1062-6050-356-19
